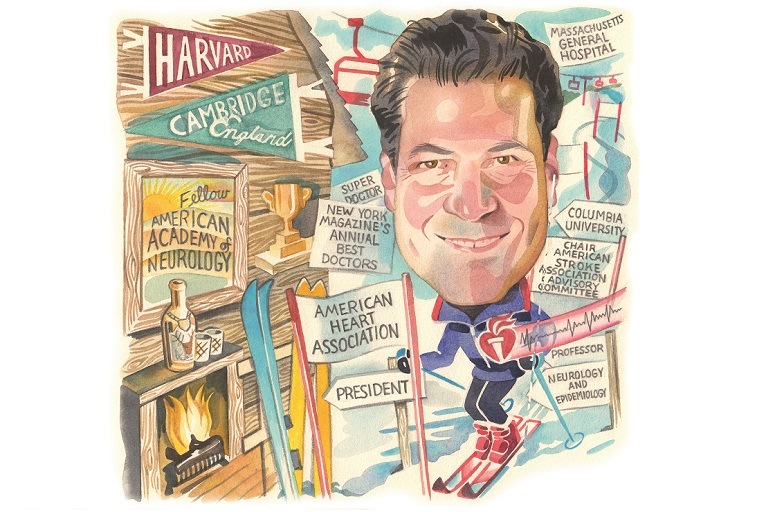
 Mitchell Elkind is a professor of Neurology and Epidemiology at Columbia University Irving Medical Center, and chief of the Division of Neurology Clinical Outcomes Research and Population Sciences (Neuro CORPS) in the Neurology Department of Columbia University, New York, USA. He is the current American Heart Association (AHA) president. Elkind talks to NeuroNews about his neurology career.
Mitchell Elkind is a professor of Neurology and Epidemiology at Columbia University Irving Medical Center, and chief of the Division of Neurology Clinical Outcomes Research and Population Sciences (Neuro CORPS) in the Neurology Department of Columbia University, New York, USA. He is the current American Heart Association (AHA) president. Elkind talks to NeuroNews about his neurology career.
What initially attracted you to medicine and neurology?
I was a reluctant medical student, but an enthusiastic neurologist! Growing up with a physician father, I felt the need to distinguish myself in some way. He was a nephrologist, and acid-base balance just did not excite me. So in college, I studied philosophy, trying to understand the meaning of life. It turned out that the most interesting aspects of philosophy, to me, were understanding the philosophy of the mind, how the brain works and what it tells us about who we are. I never figured all that out, but along the way I discovered that I wanted to take care of people with brain disorders, since neurological problems were the most informative window into people’s lives that I have found.
Who were your mentors and what impact have they had on your career?
I am fortunate to have had terrific mentors. I learned from several people who I consider to be the best neurologists in the world. C Miller Fisher at Massachusetts General Hospital described many of the syndromes of stroke that we take for granted today. He demonstrated that patience and attention to an individual patient’s story can teach us things never before seen. Walter Koroshetz shared that same passion for clinical detail, and combined it with a scientific approach. The brilliant Anne Young showed me how to do a neurological examination with style, and demonstrated what academic and scientific leadership looks like.
JP Mohr at Columbia has an incredible awareness of neurological history and the most intimate understanding of the neurological literature of anyone I have met. Ralph Sacco, the first neurologist to serve as president of the AHA, showed me the value of studying populations, as well as individual patients, as a way to best understand the causes of disease in an unbiased fashion. I learned different things from all of them, and I hope I am able to bring together their skills in meaningful
new ways.
Has COVID-19 impacted your practice and what were the lessons learned from this?
I lived through the height of the pandemic in New York City in March–April 2020, and it affected the way I think about my career and practice in many ways. I had never feared for myself and my family while practicing before, but I did then. It was almost reminiscent of the uncertainty we faced after 9/11 in New York. There was a sense of heightened awareness, and every day I learned something new. But the people who most impressed me during that period were our residents, fellows, and med students. They rose to the occasion, took on the challenges of caring for these incredibly sick patients, and risked their own lives and careers. I learned more from them than they did from me, I am certain.

What has your experience been as president of the American Heart Association during the pandemic?
Serving as AHA president during a pandemic was obviously not what I had planned for the year! I was intending to focus on expanding AHA’s work on brain health, engaging other neurologists in the work of the AHA, and increasing the research funding going to brain disease. Who knows what we will be asked to do when called to serve? I am extremely proud of the work of the AHA during my tenure. Instead of focusing only on brain stuff, I learned about COVID-19 and heart disease, worked on several COVID-19-related research projects, and tried to educate people about seeking help during the pandemic and getting their vaccines. This pandemic was not only about the coronavirus: another major area of focus for us was addressing the impact of structural racism on health disparities, a problem made even more acute by the pandemic.
What has been the most important development in the neurology field during your career?
The rapid changes in stroke care have been incredible. The acceleration of stroke care from thrombolysis in 1996, to the proven benefits of thrombectomy in 2015, to treatment in extended time windows just a few short years later, has been astounding. The fact that we can now treat stroke, and not just watch it occur, is a testament to the tireless work of so many phenomenal colleagues.
What has been the biggest disappointment?
I do feel that for all the great advances in acute stroke care, we still cannot prevent stroke as well as we should. Stroke mortality has been inching back up. Large segments of the population, including rural populations and communities of colour, do not have access to adequate care. Obesity, diabetes, and substance abuse continue to be major problems. We know what needs to be done for the most part, but social and economic barriers seem to trip us up. We need to address these problems with the same intensity that we do the technological advances.
What questions would you like to see answered in the field?
I have two major areas of interest right now. One is understanding the relationship of heart disease, like atrial fibrillation and atrial cardiopathy, to stroke risk and prevention. My colleagues and I have focused on the idea that patients with abnormalities of the left atrium can have strokes even without developing atrial fibrillation, and that anticoagulation can prevent those strokes. We are now conducting a federally-funded, international trial, called ARCADIA, testing these ideas.
The second major area is one that has excited me since the beginning of my fellowship: whether infections can cause stroke and worsen outcomes after stroke. That concept, of course, has become even more relevant since the onset of the coronavirus pandemic, since we do indeed see strokes occurring in patients with COVID-19. In a way, there is an irony that I am AHA president during this pandemic since this is something I have been exploring as an epidemiologist for the past 25 years.
Outside of your research, what has been the most interesting paper or presentation you have seen in the last year?
I think the most exciting advance of this crazy pandemic year has been the record-breaking speed of development of the mRNA vaccines for COVID-19. Within days of the virus being identified, investigators at the National Institutes of Health (NIH) and elsewhere had produced the mRNA sequences for the spike protein that would become the basis for the vaccines. Almost before the virus was on our shores, we had a vaccine ready for testing. Within less than a year, we had solid evidence that this entirely new category of vaccines worked extremely well, better than anyone had hoped. The flip side of this great scientific advance, of course, was the great failure of the USA to take the virus seriously enough until the vaccines became available, allowing rapid spread, variant mutations, and massive death and societal upheaval.
What advice would you give to those beginning their neuro career?
Find a mentor with whom you really connect. I was fortunate to have great mentors who not only taught me and modelled the highest forms of professional accomplishment, but also made opportunities available for me. Then find an area of the field that makes you excited to wake up and think about. Keep chipping at it from different angles, put your own stamp on it, and try to find others who share your passion because it is usually more fun to work with others on big projects. And be patient: big ideas generally take time to mature.
Could you tell us about a particularly memorable case you have had, and what you learned from it?
My most challenging case was a diagnostic dilemma that played out over several years. The patient was a young man who presented with episodic visual loss due to intracranial carotid stenosis, involving the ophthalmic artery, as well. After extensive evaluation, we thought he might have vasculitis, and treated him for that, but he also had some unusual immunological and haematological features, as well as a rash.
Eventually, when a family member convinced him to stop his immunosuppressive medication, he developed a rapidly progressive and ultimately fatal multisystem disorder. It turned out that he had POEMS syndrome, a rare plasma cell disorder that can be rarely associated with a paraneoplastic vasculopathy and strokes. He was especially unusual in that he presented with strokes as an initial manifestation. I was devastated that we were unable to save him. He might have been saved by an earlier bone marrow transplant. It is a humbling business. Now I always try to think of what I might be missing when things do not add up fully.
What are your interests outside of medicine?
My interests outside of medicine are enjoying nature and the outdoors, primarily in Northwest Connecticut, in whatever way the season permits: gardening in the spring, paddle boarding on our lake in the summer, hiking the hills in the fall, skiing in the winter, and after it all, enjoying a single malt while watching the sun set!
FACT FILE
Current appointments:
- Jan 2014–current: Professor of Neurology and Epidemiology in the Sergievsky Center; Columbia University College of Physicians and Surgeons; Mailman School of Public Health, Columbia University, New York, USA
- Chief, Division of Neurology Clinical Outcomes Research and Population Sciences (Neuro CORPS), Department of Neurology, Columbia University, New York, USA
Education:
- September 1983–June 1987: BA in Philosophy at Harvard College, Cambridge, USA
- September 1987–August 1988: M.Phil in History and Philosophy Science at Darwin College as a National Science Foundation Graduate Fellow, Cambridge University, Cambridge, UK.
- September 1988–June 1992: M.D., Harvard Medical School, Boston, USA
- July 1996–June 1998: M.S. in Epidemiology Columbia University School of Public Health New York, New York, USA
Honours (selected):
- American Heart Association Stroke Council Award, Chicago, 2018
- AHA/ASA Stroke Hero Award, 2019, New York City CycleNation event
- President-Elect, American Heart Association, 2019–2020
- President, American Heart Association, 2020–2021













