According to late-breaking data presented at the Society of NeuroInterventional Surgery’s (SNIS) 17th Annual Meeting, a wireless endovascular brain–computer interface (BCI) “may improve capacity to perform activities in daily living and functional independence” in patients with severe paralysis.
This conclusion was reached by Thomas Oxley (University of Melbourne, Melbourne, Australia) and Peter Mitchell (Royal Melbourne Hospital, Melbourne, Australia), who together presented the first-in-human examination of the stentrode, an implantable brain-computer interface, during the virtual meeting.
“We have demonstrated that the signal can be used to drive the mouse and keyboard to utilise Windows 10 in a patient who had failed upper limb control, and that instrumental activities of daily living may be a useful scale for BCI efficacy outcomes,” added Oxley.
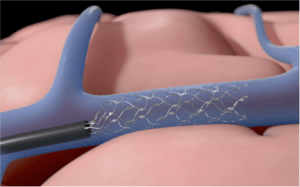
He began by telling the SNIS online audience that this technology is now eight years in the making. Oxley’s team in Melbourne have developed a stent-electrode (known as a stentrode) device that is implanted in the venous system, enabling patients with paralysis to control external devices in an attempt to improve activities of daily living.
Oxley explained that for BCIs, the hope is that the technology can assist patients that have paralysis. Paralysis can be due to a range of conditions, he noted, which can affect anywhere from the subcortex to the brainstem, to the spinal cord or the peripheral nerves.
Delving further into the background, he added: “The concept with the BCI is that if there are three elements within these patients that you have to satisfy—one is that they have preserved motor cortex (detectable on functional MRI); two is that they have an upper limb paralysis, which is assessed by a neurologist; and three, that the paralysis has resulted in a functional impairment—then a BCI may enable those patients to regain control over external devices that they could not otherwise control.”
Describing the system itself, he told viewers that it is a fully implanted intravascular array that sits in the superior sagittal sinus and records from the motor cortex. After the electrocorticography signal is detected, an algorithm is used to convert this into “intended attempted movement”, which is in turn converted into functions aimed at taking control over the mouse and keyboard. This then assists patients with upper limb paralysis to “utilise control over personal devices,” Oxley stated. “We intend to capture that clinical improvement in scales including activities of daily living.”
“This is a first-in-human study. The first patient that we are about to present is a 75-year-old male who has motor neuron disease, or ALS [amyotrophic lateral sclerosis], which is upper limb predominant, with lower motor neuron features. He is able to speak but has weakening vocal cords, and is dependent on his wife for all activities of daily living. He has been unable to independently use the telephone, computer, and do finances,” Oxley said.

The neurointervention procedure
Peter Mitchell took over to explain to the SNIS audience the implantable components of the device. “The stentrode head is a self-expanding array; 16 sensors record the signal with 4mm spacing. This is connected via the stentrode flexible lead, which passes through the venous system, and then subcutaneously, to see the Internal Telemetry Unit (ITU).”
He told viewers that the neurointervention procedure that was performed at the Royal Melbourne Hospital was first proceeded by assessing the access approach, and whether to go right or left by review of computed tomography (CT) and a structural MRI.
“Functional MRI was then used to identify the motor cortex and allow co-registration to DSA [digital subtraction angiography] targeting during the procedure,” Mitchell noted, adding that the jugular vein access and superior sagittal sinus deployment was via a percutaneous direct puncture, and retrograde catheterisation of the superior sagittal sinus was done using a benchmark guide catheter system.
According to Mitchell, the team was able to place the device within 1mm, and a stable stent and lead position were confirmed at three months. There was no evidence of complication, he added, as no thrombosis or stenosis was observed at three months.
Preclinical work
Oxley confirmed that the team carried out “a lot” of animal work leading up to this first-in-man study. He said: “The majority of the work laid out by the US FDA [Food and Drug Administration] was to demonstrate safety around thrombosis.”
The main learning from this, according to Oxley, was that endothelialisation was the biggest determinant of thrombosis. “We demonstrated that in animal studies, 95% device endothelialisation in the sinus occurred after 45 days. For that reason, we have pursued a dual-antiplatelet therapy out to 90 days, and a single agent beyond 90 days,” he confirmed.
Decoding motor intent
Once the device is in and turned on, Oxley explained that a training exercise is undertaken with the patient, to identify different attempted types of movement. These can include left, right, ankle, and quad-movements, he posited. Following this, the machine learning algorithm is trained to classify these particular movements. “Then, we turn those into inputs on a mouse or a keyboard,” Oxley told the audience.
“For our first patient, he was still able to use eye-tracking for the cursor, so we utilised the first several outputs for left-click or zoom functioning, which in combination with his eyes, gave him control over Windows 10, and he was able to regain function.”
Assessing performance
“The way we assessed the performance was primarily around typing,” Oxley asserted. The team evaluated selection accuracy (click accuracy), which the patient was averaging at around 91%.
Oxley said that the patient was selecting keys on the keyboard to type at a correct-characters per minute rate of 13. “He utilised the system to conduct text messaging, emailing, online shopping, and online banking, which he was unable to do before. This resulted in an improvement in his activities of daily living.”
Next, Oxley displayed a video of the patient sending his wife a text message. “He was not able to do this before,” he argued, adding that his wife always had to be there. “She is now able to leave the house because he can access her via WhatsApp by opening the app and sending her a message.”
A future for stentrode
Concluding the presentation, Oxley told the online viewers: “This is obviously only the first patient; we have a lot of work to do.”
He argued that the team are not making any claims on safety yet, and put forward that they have approval to implant the stentrode in five more patients in Melbourne, which they are currently moving through. “We are looking at outcomes that we have agreed upon with the FDA, including three- and 12-month thrombosis and change in vessels. In our first patient, we have three and six-month data, and there has been no stenosis.”
Lastly, Oxley confirmed that the next steps are to launch a feasibility study—also in the USA—and then within three years “to hopefully launch a pivotal trial to demonstrate this technology in a subset of patients with paralysis”.
For more stories from SNIS 2020, click here.













